October is National Eczema Awareness Month so let’s spread awareness starting with some basic facts.
What is Eczema?
We asked our board certified dermatologist, Dr. Michelle Cihla. She explained, “eczema is a skin condition that causes the skin to become red, itchy and inflamed. It commonly appears as dry or scaly patches and can develop anywhere on your body. It isn’t contagious, but develops because of a combination of environmental triggers and genetics.”
FACT: Eczema is very common, with over 30 million Americans having some type of this skin condition.
What Are the Types of Eczema?
- Atopic dermatitis – This type is caused by a malfunction in the immune system and problems with the skin barrier.
- Contact dermatitis – When skin touches a known irritant and/or allergen, it can cause this type of eczema.
- Dyshidrotic eczema – Exposure to allergens causes this kind eczema, which presents itself as itchy blisters on the feet and hands.
- Hand eczema – This type is caused by a combination of genes, irritants and/or allergens.
- Lichen simplex chronicus – Too much scratching and rubbing lead to this type of eczema, which presents as thick, scaly patches on the skin.
- Nummular eczema/discoid eczema/nummular dermatitis – Allergens or very dry skin cause this kind of eczema to develop. It manifests as round lesions and can weep fluid. You will find this type of eczema most commonly in older populations.
- Seborrheic dermatitis – This form of dermatitis appears as white or yellow flaky, greasy patches in places with more oil-producing glands. A combination of genetics, hormones and microorganisms on the skin all contribute to the development of this type of eczema. In addition, “cradle cap” is the common name for this skin condition in infants.
- Stasis dermatitis – This kind of eczema occurs when poor circulation to the legs causes the veins to swell and leak fluid. As a result, swelling, skin redness, as well as itch may occur.
Treating Eczema – Get the Facts
Living with eczema can be an ongoing challenge, but the condition is manageable. This is largely due to the various treatment options that are now available. For example, your dermatologist may recommend: prescription topical medications, phototherapy and/or biologics. However, your dermatologist will consider your age and the severity of your case before making any recommendation.
According to Dr. Cihla,
“if you are affected by eczema it is best to know your triggers to avoid exposure. Be consistent with your treatment plans and develop a daily moisturizing regimen to help soothe dry skin.”
In conclusion, if you are struggling with eczema or other skin issues and don’t know where to turn, we can help. Our board certified experts are available at three convenient locations in Kentucky. Call a local dermatologist today!






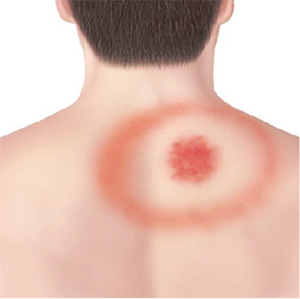 Other early symptoms of Lyme disease include flu-like symptoms, low-grade fever, fatigue, headaches and muscle or joint aches and pains. Later stages of the disease don’t develop until weeks or many months later. Many complications can follow an untreated case of Lyme disease. These include meningitis (stiff neck, headaches, vomiting, fever), Bell’s palsy (paralysis of part of the face), heart block and irregular heartbeats, painful joints, muscles and bones. Lyme disease is diagnosed based on symptoms, physical exam with your dermatologist and probability of exposure to infected ticks. Laboratory testing can be helpful, but only if used and interpreted correctly and performed with validated methods. Early treatment typically consists of orally administered antibiotics.
Other early symptoms of Lyme disease include flu-like symptoms, low-grade fever, fatigue, headaches and muscle or joint aches and pains. Later stages of the disease don’t develop until weeks or many months later. Many complications can follow an untreated case of Lyme disease. These include meningitis (stiff neck, headaches, vomiting, fever), Bell’s palsy (paralysis of part of the face), heart block and irregular heartbeats, painful joints, muscles and bones. Lyme disease is diagnosed based on symptoms, physical exam with your dermatologist and probability of exposure to infected ticks. Laboratory testing can be helpful, but only if used and interpreted correctly and performed with validated methods. Early treatment typically consists of orally administered antibiotics.